Mayo Clinic physicians map patients’ brain waves to personalize epilepsy treatment
Research News
|
Nov 20, 2025



DBS involves implanting electrodes in the brain to deliver electrical pulses that help prevent and control seizures. While effective, DBS is typically administered with electrodes placed in the same brain region across most patients. Mayo Clinic physician-scientists are now tailoring the treatment to an individual's seizure network before DBS placement.
"Our unique approach aims to tailor neuromodulation for each patient," says Nick Gregg, M.D., a Mayo Clinic neurologist and lead author of a paper published in the Annals of Neurology. "We're moving away from one-size-fits-all to an individualized approach that maximizes seizure network engagement to better modulate abnormal brain wave activity."
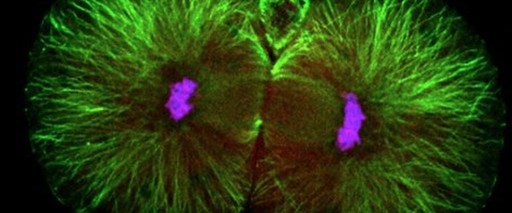
Once researchers identify the specific area in the thalamus — a small relay hub deep within the brain — that connects to a patient's seizure network, they can fine-tune stimulation settings for that individual. Because seizures occur infrequently, clinicians analyze erratic brain wave patterns that signal abnormal activity.
"We're trying to disrupt the pathological hypersynchrony and reduce network excitability to lower seizure risk," says Dr. Gregg.
Ten patients received this personalized approach while being evaluated for epilepsy surgery. The next phase of research will follow those who have since received permanent DBS implants using this personalized approach.
This research is part of Mayo Clinic's Bioelectronics Neuromodulation Innovation to Cure (BIONIC) initiative, which unites clinical insight with cutting-edge engineering to deliver novel diagnostics and therapies. Through intellectual property development, strategic partnerships and patient-centered trials, BIONIC transforms innovation into impact — advancing care for complex neurological conditions.
Dr. Gregg's research was supported by the Tianqiao & Chrissy Chen Institute. Review the study for a complete list of authors, disclosures and funding.
DBS involves implanting electrodes in the brain to deliver electrical pulses that help prevent and control seizures. While effective, DBS is typically administered with electrodes placed in the same brain region across most patients. Mayo Clinic physician-scientists are now tailoring the treatment to an individual's seizure network before DBS placement.
"Our unique approach aims to tailor neuromodulation for each patient," says Nick Gregg, M.D., a Mayo Clinic neurologist and lead author of a paper published in the Annals of Neurology. "We're moving away from one-size-fits-all to an individualized approach that maximizes seizure network engagement to better modulate abnormal brain wave activity."
Once researchers identify the specific area in the thalamus — a small relay hub deep within the brain — that connects to a patient's seizure network, they can fine-tune stimulation settings for that individual. Because seizures occur infrequently, clinicians analyze erratic brain wave patterns that signal abnormal activity.
"We're trying to disrupt the pathological hypersynchrony and reduce network excitability to lower seizure risk," says Dr. Gregg.
Ten patients received this personalized approach while being evaluated for epilepsy surgery. The next phase of research will follow those who have since received permanent DBS implants using this personalized approach.
This research is part of Mayo Clinic's Bioelectronics Neuromodulation Innovation to Cure (BIONIC) initiative, which unites clinical insight with cutting-edge engineering to deliver novel diagnostics and therapies. Through intellectual property development, strategic partnerships and patient-centered trials, BIONIC transforms innovation into impact — advancing care for complex neurological conditions.
Dr. Gregg's research was supported by the Tianqiao & Chrissy Chen Institute. Review the study for a complete list of authors, disclosures and funding.